The potential impact of COVID-19-related disruption on tuberculosis burden
This study has not yet been peer reviewed.
The COVID-19 pandemic has the potential to increase the burden of TB through disruptions to health services, or to decrease it through reduced social contact, and therefore transmission. The overall impact on TB depends on the balance between health service disruption and social distancing. We used a mathematical model to investigate this.
Over five years, the potential benefit of social distancing on TB burden is likely to be larger for TB disease incidence than for TB deaths. In scenarios with substantial health service disruption, we projected an increase in both TB cases and deaths, regardless of the level of social distancing. As many as 200,000 additional TB deaths could occur in China, India, and South Africa over the next five years, as a result of COVID-19-related disruptions.
Any benefit of social distancing on TB deaths is likely to be outweighed by health service disruption. As such, it is crucially important to maintain and strengthen TB-related health services during, and after, the COVID-19 pandemic.
Read the published letter here.
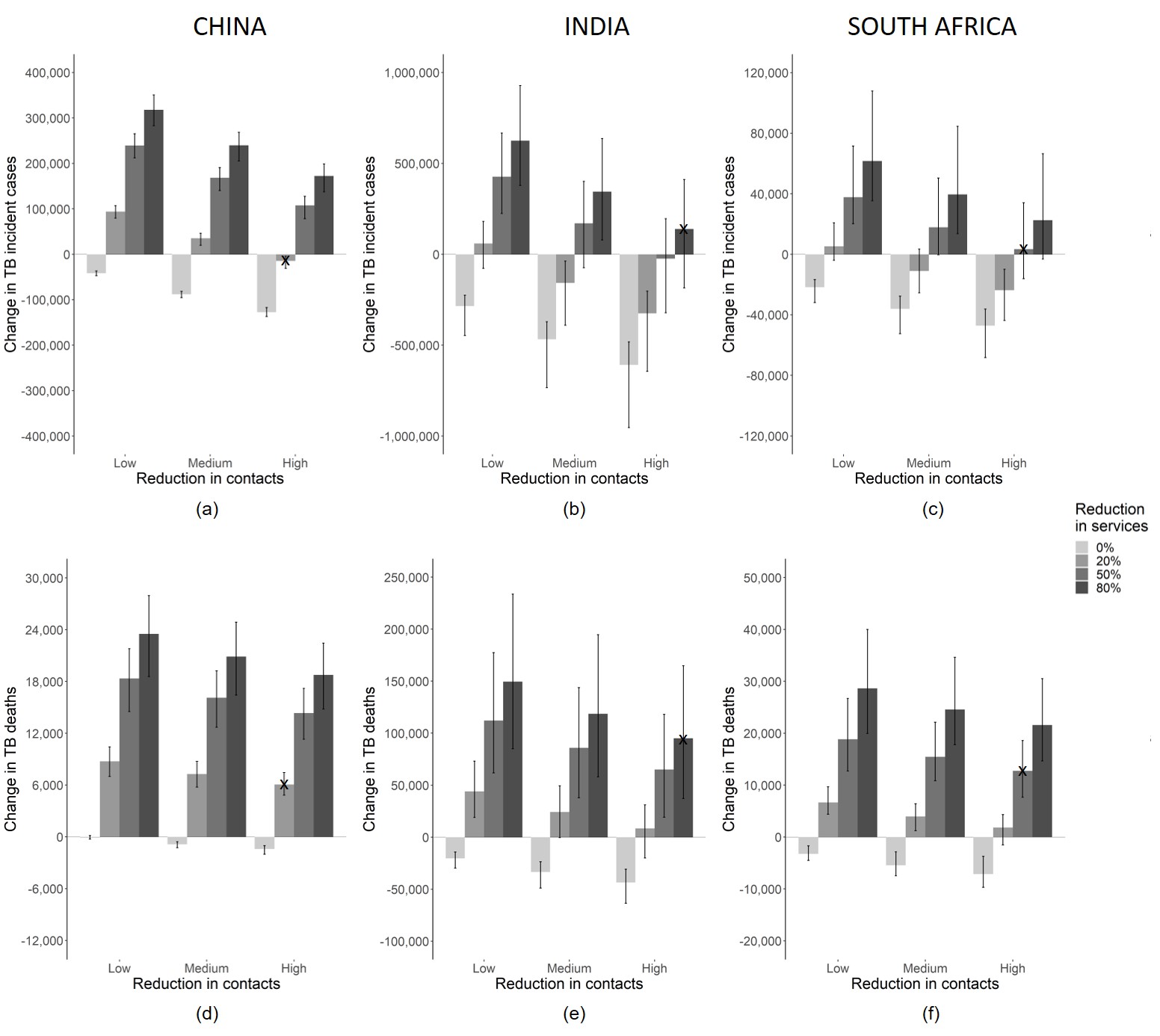 Figure 1: Cumulative change in TB (a-c) incidence and (d-f) deaths over 5 years as a result of social and/or health system disruption due to the COVID-19 pandemic for (a,d) China, (b,e) India and (c,f) South Africa. Results show the median of model runs, while whiskers denote the range of run results. Small black crosses indicate author assessment of most plausible scenarios based on current anecdotal information. Note y-axes scales differ by country and indicator.
Figure 1: Cumulative change in TB (a-c) incidence and (d-f) deaths over 5 years as a result of social and/or health system disruption due to the COVID-19 pandemic for (a,d) China, (b,e) India and (c,f) South Africa. Results show the median of model runs, while whiskers denote the range of run results. Small black crosses indicate author assessment of most plausible scenarios based on current anecdotal information. Note y-axes scales differ by country and indicator.