Rapid testing strategies for traced contacts: comparing quarantine, quarantine and testing, and repeat daily testing
This study has not yet been peer reviewed.
You can download a copy of the full report here.
- Traced contacts of confirmed SARS-CoV-2 cases in the UK are currently asked to quarantine until 14 days have passed from their last exposure to the index case to avert onwards transmission of SARS-CoV-2.
- Here we assess the merit of using lateral flow antigen (LFA) tests to allow for a shorter quarantine period by testing at its end, or to replace quarantine altogether by testing daily upon tracing and isolating only when test-positive.
- We use an agent-based model of SARS-CoV-2 infection to simulate an exposed contact’s contact tracing delay, incubation period, probability of becoming symptomatic, infectivity profile, and time-varying probability of detection with PCR and LFA.
- We find that testing on day 7 post-exposure with LFA may avert 46% (95% UI: 26, 64%) of onward transmission compared to 47% (95% UI: 30, 62%) with a 14-day post-exposure quarantine period with no testing, assuming a 3 day delay from testing of the index case to isolation of contacts, 50% of contacts fully adhering to quarantine, and 67% of contacts fully adhering to post-symptom or post-positive test isolation.
- If contacts are not required to quarantine, but instead undergo daily LFA tests for the 5 days after they are traced, 44% (95% UI: 23, 66%) of transmission may be prevented, accounting for current Test and Trace delays.
- Daily repeated lateral flow testing may allow for the requirement to quarantine to be removed with a small increase in transmission risk, which could itself be offset by increased participation and adherence to isolation. As LFA testing reportedly has high sensitivity at high viral loads, cases may be detected and isolated as soon as they become infectious, averting subsequent transmission.
- However, the amount of transmission averted from secondary infections is limited by the delay from testing of the index case to isolation of contacts, and by the proportion of contacts who adhere to quarantine and self-isolation. By comparison, the potential loss in programme effectiveness through switching from a policy of 14 day quarantine to 7 day quarantine with a subsequent LFA test, or daily LFA testing upon tracing, is small.
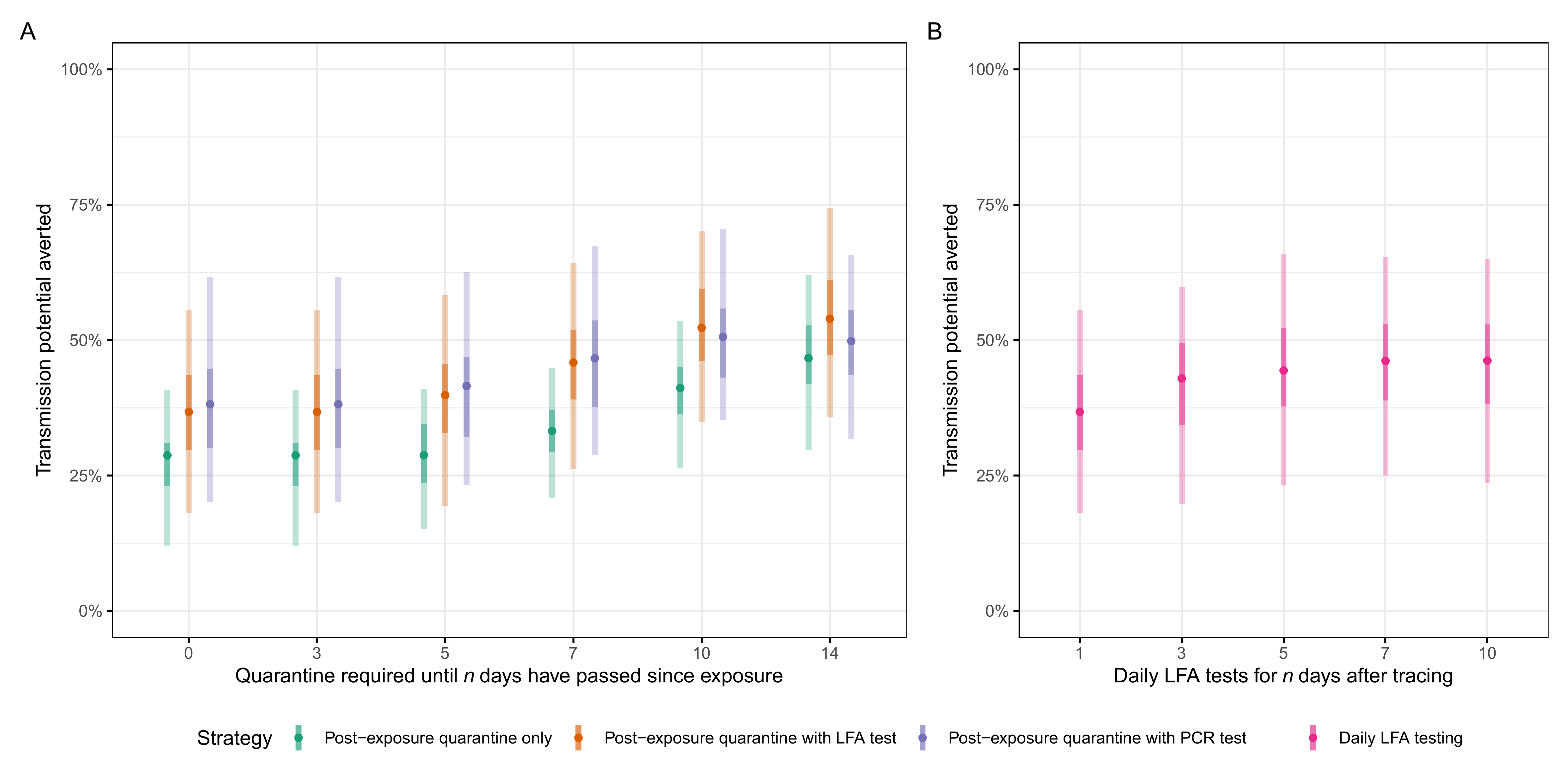
Figure: Transmission potential averted (integral of infectivity curve over time spent in quarantine or isolation) for each strategy, with quarantine-based strategies (quarantine required from time of tracing until n days have passed since exposure, either with or without a test on the final day) in A and daily testing strategies (daily lateral-flow antigen tests without quarantine for n days from tracing, isolating only upon a positive test result) in B. Quarantine adherence assumed to be 50% prior to symptom onset or a positive test result, where adherence is assumed to increase to 67%. The delay from index case’s positive test until the tracing of secondary cases is assumed to be 3 days (current average) (4). Time-varying values of sensitivity of LFA given by scaling the corresponding PCR value by 0.739. Central bars indicate the median amount of transmission potential averted for a given strategy, with 95% and 50% uncertainty intervals indicated by light and dark shaded bars, respectively. Here PCR tests (purple) are shown on the day of sampling, however the return of a result would take 1-2 days, and hence some additional transmission would be averted while awaiting a test result. For other assumptions of symptomatic self-isolation rates, and test and trace delays, see Figure S2 and S3.